Cardio Test INFAI®
Lipoprotein analysis in serum for risk assessment of cardiovascular diseases. The test is evaluated by NMR spectroscopy.
Lipoproteins and cardiovascular disease
Lipoproteins do not appear as clearly distinguished, standardized classes, but form a continuum from small and dense particles to large and less-dense ones. Upon closer inspection, lipoproteins can be divided into categories referred to as lipoprotein subclasses (also referred to as subfractions). These subclasses are distinguished not only by size, density and composition, but also by their atherogenicity. The importance of measuring LDL and HDL in determining cardiovascular risk is undisputed nowadays. Both parameters are used for indication of possible treatment with statins and for treatment control. In Germany, enzymatic tests that measure the cholesterol content of lipoproteins (LDL-C and HDL-C) are used for this. For LDL-C, there are recognized intervention limits for treatment with statins, as well as target ranges for treatment monitoring, based upon which more intensive statin treatment may recommended. Gottlieb A, Leven AS, Sowa JP, Borucki K, Link A, Yilmaz E, Aygen S, Canbay A, Porsch-Özcürümez M. (2020): Lipoprotein and Metabolic Profiles Indicate Similar Cardiovascular Risk of Liver Steatosis and NASH. Digestion.1-11; doi: 10.1159/000510600.
Why should lipoprotein subclasses be measured?
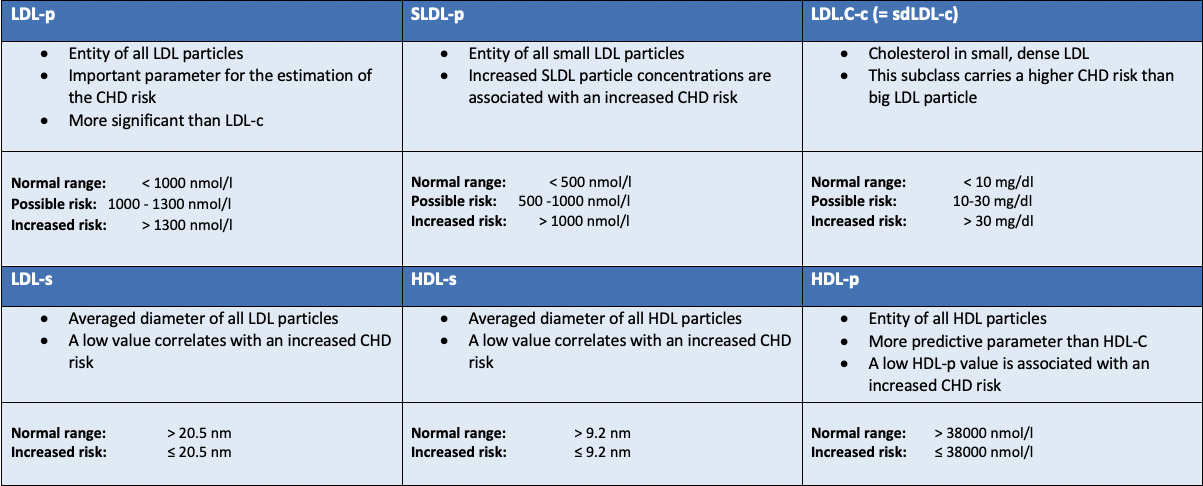
Lipoprotein subclasses are becoming increasingly important as risk factors for cardiovascular disease (CVD). The relationship between cholesterol in lipoprotein subclasses, particle concentration, particle size and CVD has been proven in a series of studies. Within the LDL fraction, small LDL particles in particular are positively associated with CVD risk. For several years, now, it has been recognized that enzymatic tests are not optimal predictors of cardiovascular risk. This is partly due to the fact that the traditional test measures the cholesterol fraction of LDL particles. As a result, small LDL particles (sdLDL particles) are under-represented, even though particularly high cardiovascular risk has been attributed to this specific subclass. This is why the number of LDL particles (LDL-P) in particular is a significantly better predictor of cardiovascular risk.
Which patients should be tested?
In general all patients would benefit from the new measurement method. Depending on the decision limit for treatment, it is generally expected that 10–30 % could be assigned to a different risk group, which could potentially result in the selection of a treatment option. The calculated benefit for patients increases as the risk of atherosclerosis rises. However, there is not yet a clear recommendation from a professional association regarding which patients the new test should be used on.
From our point of view, it seems particularly beneficial to use it in younger patients with a suspected family history and for whom early treatment is considered. In addition, an examination should at least be considered for patients with a higher risk of atherosclerosis, e.g. with known CHD or diabetes mellitus. Due to the shifting of LDL sub-fractions, treatment monitoring with the help of the new test should at least be considered in selected patients.
How does the new test work and why is it more accurate?
With our modern SampleJet automation technology, we can measure up to 200 serum samples fully-automatically in 24 hours using high flux throughput. Integrated sample cooling to 2–8 °C minimizes common ageing processes and thus increases the quality and reliability of the analysis results obtained. Fully-automatic processing and evaluation gives us up to 29 parameters for optimum assessment of a potential risk for myocardial infarction.By analyzing the different resonance frequencies in the ¹H spectrum, conclusions can be drawn about the molecules examined and the supramolecular particles (such as lipoproteins). This allows for highly detailed analysis of the different lipoproteins. It is possible to not only determine the proportion of HDL, LDL, VLDL and IDL, but also to further subdivide the fractions into large and small particles.
Downloads
More information
More information
References
- Gottlieb, A., Leven, A. S., Sowa, J. P., Borucki, K., Link, A., Yilmaz, E., Aygen, S., Canbay, A., & Porsch-Özcürümez, M. (2021). Lipoprotein and Metabolic Profiles Indicate Similar Cardiovascular Risk of Liver Steatosis and NASH. Digestion, 102(5), 671–681.
- Potočnjak, I. et al., Serum Concentration of HDL Particles Predicts Mortality in Acute Heart Failure Patients. Sci Rep, 2017; 7:46642.
- Kontush, A. et al., HDL particle number and size as predictors of cardiovascular disease. Front Pharmacol, 2015; 6(218):1-6.
- Williams, P.T. et al., Comparison of four methods of analysis of lipoprotein particle subfractions for their association with angiographic progression of coronary artery disease. Atherosclerosis 2014; 233(2):713-720.
- Toth, P.P. et al., Cardiovascular risk in patients achieving low-density lipoprotein cholesterol and particle targets. Atherosclerosis 2014; 235:585-591.
- Folse, H.J. et al., Clinical- and cost-effectiveness of LDL particle-guided statin therapy: A simulation study. Atherosclerosis 2014; 236:154-161.
- Mora, S. et al., Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events. Circulation 2014; 129(5):553-561.
- Cole, T. et al., Association of apolipoprotein B and nuclear magnetic resonance spectroscopy-derived LDL particle number with outcomes in 25 clinical studies: assessment by the AACC lipoprotein and Vascular Diseases Division Working Group on Best Practices. Clin Chem 2013; 59:752-70.
- Garber, A.J. et al., AACE comprehensive diabetes management algorithm, Endocr Pract 2013; 19:327-36.
- Stone, N.J. et al., 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. JACC 2013; 63(25):2889-934.
- deGoma, E.M. et al., Discordance between non-HDL-cholesterol and LDL-particle measurements: Results from the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis 2013; 229:517-523.
- Mora, S. et al., High-Density Lipoprotein Cholesterol, Size, Particle Number, and Residual Vascular Risk After Potent Statin Therapy. Circulation 2013; 128:1189-1197.
Studies
Study number: LipoNMR 14/D/16 Start 2017 Duration 2018-2019
Bewertung der Effektivität ausgewählter Aphereseverfahren anhand der Veränderungen von Lipoproteinfraktionen und Subfraktionen vor und nach Lipoproteinapherese bei Patienten mit Fettstoffwechselstörung mittels NMR-Spektroskopie sowie des etablierten photometrisch-kinetischen Standardverfahrens. Sponsor: INFAI
